Discovery of a protein that causes early dementia. Scientists at the MRC Molecular Biology Laboratory have succeeded in identifying a protein that plays a major role in early-onset dementia and could revolutionize the diagnosis and treatment of this disease.
Discovery of a protein that causes early dementia
According to SD, scientists at the MRC Molecular Biology Laboratory have identified protein aggregations known as TAF15 as a key factor in frontotemporal dementia, a discovery that could revolutionize the diagnosis and treatment of this disease.
This study also investigates the potential involvement of TAF15 in both frontotemporal dementia and motor neuron disease.
Therefore, the researchers of this laboratory have created the first potential therapeutic target for a form of early dementia.
Most neurodegenerative diseases, including dementia, are caused by proteins that accumulate in strands called amyloids.
In most of these diseases, researchers have identified proteins that accumulate, allowing them to target these proteins for diagnostic tests and treatments. But in about 10% of cases of frontotemporal dementia, scientists have not yet identified the rogue protein that causes it.
Now scientists have identified the TAF15 protein aggregate structures as the cause of this disease.
The nature of frontotemporal dementia
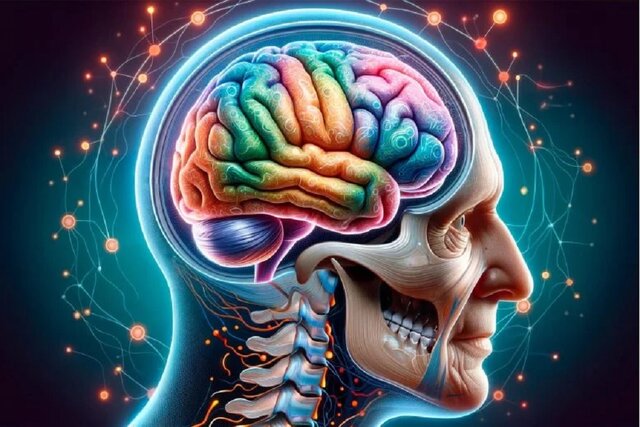
Frontotemporal dementia is caused by damage to the frontal and temporal lobes of the brain, which control emotions, personality, and behavior, as well as speech and word comprehension.
The disease usually starts at a younger age than Alzheimer’s disease and is most often diagnosed in people between the ages of 45 and 65, although it can affect younger or older people as well.
In an article recently published in the journal Nature, research led by scientists at the Medical Research Council (MRC) Molecular Biology Laboratory in Cambridge, UK, has identified protein aggregation structures that could be a target for the future development of diagnostic tests and treatments.
Advances in molecular understanding
Dr Benjamin Riskeldi-Falcon, who led the study at the MRC Laboratory of Molecular Biology, said: “This discovery changes our understanding of the molecular basis of frontotemporal dementia. This is a rare finding of a new member of a small group of proteins that accumulate in neurodegenerative diseases.
He added: “Now that we have identified this key protein and its structure, we can target it to diagnose and treat this type of dementia, exactly the same as the strategies currently used to target the entire amyloid beta and tau proteins that The symptoms of Alzheimer’s disease are in progress.
Advanced techniques reveal new insights
Scientists used advanced cryo-electron microscopy (cryo-EM) to study protein clumps from donated brains of four people with this type of frontotemporal dementia at atomic resolution.
Scientists have long thought that a protein called FUS builds up in this type of dementia, based on similarities it has with other neurodegenerative diseases.
Using advanced cryo-electron microscopy, researchers at the MRC Molecular Biology Laboratory were able to determine that the protein aggregates of each brain have the same atomic structure, and surprisingly, this protein was not FUS, but another protein called TAF15.
Dr. Stephen Teter from the MRC’s Laboratory of Molecular Biology, who is the lead author of the paper, said: “This is an unexpected result because, before this study, TAF15 was not known to form amyloid fibrils in neurodegenerative diseases and no structure of this protein was available. did not have.
“Advanced cryo-electron microscopy is changing our understanding of the molecular pathology of dementia and neurodegenerative diseases more broadly by providing insights beyond the capabilities of our previous technologies,” he added.
“The technical challenge of doing this with advanced cryo-electron microscopy meant we could only look at the brains of four people,” says Dr Riskeldi-Falcon. However, now that we know this key protein and its structure, we have the potential to develop tools to screen these abnormal protein clumps in hundreds of patient samples to test how widespread they are.
Read More: Viruses against superbugs
Discovery of a protein that causes early dementia
Frontotemporal dementia and Lou Gehrig’s disease
Some people with frontotemporal dementia also have Lou Gehrig’s disease, or motor neuron disease, which is a condition in which people gradually lose control of their muscles.
In this study, two of the people who donated their brains had symptoms of both diseases and for these people, the researchers identified the same TAF15 aggregate structure in brain regions associated with motor neuron disease.
The presence of identical TAF15 clusters in two individuals with frontotemporal dementia and symptoms of motor neuron disease raises the possibility that TAF15 may play a role in both diseases, says Dr. Riskeldi-Falcon.
He added: “We are currently studying whether there is aberrant accumulation of TAF15 in people who only have motor neuron disease and do not have frontotemporal dementia.”
Dr Charlotte Durkin, Chair of the Molecular and Cellular Medicine Board at the Medical Research Council, said: “Decades of world-leading research at the MRC Molecular Biology Laboratory led to the development of advanced cryo-electron microscopy, which won Dr Richard Henderson the 2017 Nobel Prize.
He added: This latest study, which identifies a protein associated with a type of frontotemporal dementia, continues our center’s success in elucidating protein structures associated with dementia by advanced cryo-electron microscopy.
In the end, he said: knowing the identity and main structure of these fibers in this rare form of early dementia is crucial for the development of early diagnostic tests and drugs to combat their formation.
The study was funded and supported by the Medical Research Council, Alzheimer’s Research England, the US National Institutes of Health, the Alzheimer’s Association, the Frontotemporal Dementia Association, and the Swiss National Science Foundation.



 Technology9 months ago
Technology9 months ago


 Technology10 months ago
Technology10 months ago


 Technology9 months ago
Technology9 months ago


 Technology11 months ago
Technology11 months ago


 AI1 year ago
AI1 year ago

 Humans1 year ago
Humans1 year ago


 Technology10 months ago
Technology10 months ago


 Technology11 months ago
Technology11 months ago