Health
Researchers come close to reach human hibernation
Published
1 year agoon


Scientists are about to find a way to put humans into hibernation; Maybe this is the only way for humans to reach Mars.
One day in 1992, neuropharmacologist Kelly Drew was working in a laboratory at the University of Alaska Fairbanks near the North Pole when his colleague Brian Barnes, a professor of animal physiology, changed the course of his life and possibly humanity forever. Gave Barnes told Drew to reach out and brace himself for an exciting surprise. A few moments later, a sleeping arctic squirrel was in Drew’s hands. This squirrel was tightly curled up like a bullet, and its body was so cold that Drew thought it was dead, But Barnes happily told him that the frozen squirrel was in perfect health.
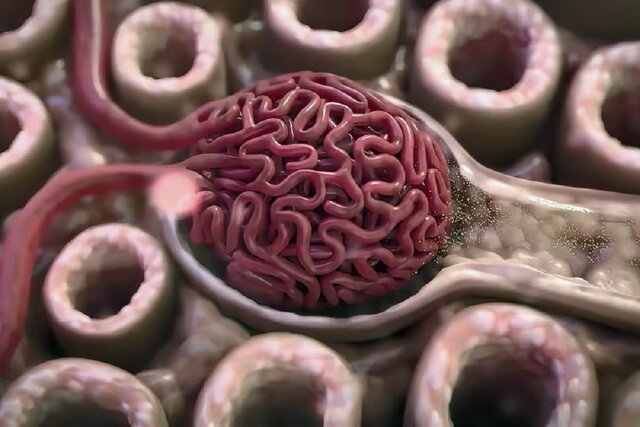
The polar ground squirrel, which had settled in the palms of Drew’s hands, had fallen into hibernation. This small animal, which holds the record for the longest hibernation, spends eight months of the year in hibernation, and during all this time, the internal temperature of its body reaches below minus 3 degrees Celsius; His brain waves become so weak that they are barely noticeable, and his heart beats only once per minute. However, it is completely alive and healthy, and with the arrival of spring, it can raise its body temperature to 37 degrees in a few hours and resume its normal life.
On that fateful day, a big question stuck in Drew’s mind; What is going on in the brain of the polar squirrel that allows it to survive in these harsh conditions? And this question started thirty years of research to bring humans a few steps closer to achieving hibernation and reaching Mars.
The big problems of traveling to Mars
Currently, three major organizations, including NASA, China National Space Agency, and SpaceX, are in a breathtaking competition to send the first human to Mars by 2040; But to win this competition, they need to solve a series of challenging problems first.
The most important problem facing the engineers who are trying to open our feet of us humans to the red soil of Mars is that we need a lot of care and maintenance. We, warm-blooded animals with high-functioning brains, burn large amounts of food, water, and oxygen during the day to survive. This high consumption makes it extremely difficult to design a light spacecraft suitable for a round trip to a planet 226 million kilometers from Earth. . By examining the eating habits of the astronauts of the International Space Station, it can be estimated that a four-member crew needs at least 11 tons of food to complete the 1100-day round trip mission to Mars. The weight of this food alone is about ten times more than that of the Perseverance rover, the largest cargo ever to reach Mars. Now, to these 11 tons of food, add all the other essentials, including the equipment needed to settle on Mars, so that the weight of a spacecraft when it leaves the Earth’s atmosphere for Mars is easily more than 330 tons, that is, more than the weight of two blue whales. Mature, go beyond. As you read this, it’s impossible to imagine where such a gigantic spacecraft will get the fuel it needs to make the round trip to Mars.


If you’ve read Arthur C. Clarke’s science fiction novels or at least seen Stanley Kubrick’s “2001: A Space Odyssey,” you can guess the solution to the spacecraft’s weight problem; That we need to reduce the crew’s metabolism to such an extent that they only need to use minimal resources during their 1,100-day journey. In the movie Space Odyssey, we see astronauts hibernate in coffin-like chambers, and in this state, their hearts beat only three times per minute. Their body temperature is slightly below 3 degrees Celsius.
John Bradford, one of the chief executives of SpaceWorks, the Atlanta-based engineering firm that manages NASA’s ambitious research projects, has devoted a large part of his 21-year career to answering the question of what allowed Kubrick as an artist. Ignore it in his film; How exactly can we safely “shut down” the human body so that it is only one step away from death and then be able to revive it whenever we want?
In search of answers
In the first days of his research, Bradford thought of hypothermia therapy as a way to turn off the human body. Hypothermia therapy is a medical technique that lowers the body temperature of people who have suffered a cardiac arrest, usually by injecting cooling fluids to 32 degrees Celsius. As the internal temperature decreases, the body’s metabolic rate decreases to such an extent that the cells can continue to work with approximately 30% less energy and oxygen, thus giving the damaged tissues a chance to repair.
Patients are usually only kept hypothermic for a day or two, as the cold causes severe shivering that can only be controlled with sedative injections and strong neuromuscular blocking drugs. However, Bradford was able to identify a few rare cases in which patients remained hypothermic for up to two weeks. This issue sparked this question in his mind: Why can’t we keep the human body in hypothermia for more than two weeks, and how long can we keep the coma?
In 2013, Bradford convinced NASA’s Advanced Innovative Concepts to fund a project to make human hibernation possible. Bradford told them that if the astronauts could be kept frozen for most of the trip to Mars, their vital resources could be reduced by 60 percent. He also hypothesized that hibernation could protect astronauts from serious physical and mental harm, from harmful radiation to the psychological dangers of isolation and extreme boredom.
A drug that suppresses shivering stops breathing


But a fundamental problem was still there; Medicines used to stop shivering frozen people also stopped them from breathing. Thus, sleeping astronauts must breathe through tubes inserted into their trachea for weeks or months. In addition, using the serum to inject fluids into the body was frightening because the syringe needle increased the possibility of infection in astronauts.
The ideal and dream way to solve this problem was to use a pill to fall into a long sleep and be able to breathe without the need for a tube. Although this extraordinary method seems science fiction, some aspects of it were familiar to Bradford; Because many animal species go to sleep for a long time every winter, and in the state of unconsciousness, their body’s desire for food and oxygen is greatly reduced. When these animals return to their alert state in the spring, they show no signs of muscle atrophy, malnutrition, or other diseases caused by prolonged immobility. Bradford concluded that it is possible to discover the secret of their hibernation by observing and examining these animals.
The beginning of NASA’s hibernation research
And so it happened that Bradford went to the very small community of hibernation researchers, Scientists who had devoted most of their lives to the study of bears, bats, and lemurs, whose hibernation was an essential part of their survival. Their research focused on the molecular changes of these hibernating animals and the reduction of their body metabolism. Since many hibernators are genetically close to us, it is possible that by changing our brains and bodies, we can also hibernate.
By the time Bradford decided to enlist the help of hibernation researchers, Kelly Drew of the University of Alaska had been researching the arctic ground squirrel for more than 20 years. When Bradford first contacted him in 2015, Drew had just made a major discovery and taken the critical first step toward giving humans the power of optional on/off.
When his colleague Brian Barnes put a frozen arctic squirrel in his hands, Drew began studying this animal using the microdialysis technique. In this procedure, small tubes are placed under the living creature’s skull to sample the brain’s neurochemicals, and usually, a wound is created where the tubes enter the skull. However, Drew was amazed at the absence of scarring in the sleeping squirrels after microdialysis. This gave him the idea of the protective properties of hibernation. “Hibernation seemed to protect the brain from damage,” he says.
The discovery of the protective properties of hibernation in animals made Drew’s research more vital in finding a way to induce hibernation in humans.


The main obstacle to the realization of winter sleep in humans is the heart’s sensitivity to rapid temperature changes.
During his time in Fairbanks, Hauck became fascinated with the study of bears. In 1960, he published a paper entitled “Possible Use of Hibernation in Space Travel,” in which he pointed out, for the first time, in precise and scientific detail how the fledgling US space program could benefit from his research. Huck said in this article that winter sleep is just a few steps away, and the main obstacle to its realization is the sensitivity of the human heart to rapid temperature changes.
Hibernations have learned how to overcome this sensitivity, and several labs are currently investigating ways to implement this in humans.
In this article, Hawk also mentioned the potential of hibernation to slow down the aging process.
Because they use much less energy during the year, hibernators live longer than mammals of the same size that do not hibernate.
Hawk estimated that if humans, like bears, could keep their internal body temperatures about 13 degrees cooler than normal, “the aging process would occur at half the normal rate.”
In the early 1960s, Hawk and his colleagues exposed a species of large squirrels called marmots that were hibernating to sudden extreme cold. They discovered that marmots’ brown fat, also present in the human body, produces heat in response to this extreme cold. Hawk research team concluded that brown fat, which warms the body by burning energy stored in cells, could be the secret to humans surviving in the frozen state of hibernation.
But Hawk died in a tragic accident in 1970, and as the Cold War got colder, hibernation research fell out of fashion. With the Pentagon and NASA cutting off funding for this research, biologists looked at hibernation as a field without a future. And since it takes a year to collect data on an animal’s hibernation cycle and compare it to their normal physical activity, research in this area is painfully slow.
However, Kelly Drew was so fascinated by the arctic ground squirrel that he dedicated several decades of his life to research on animal hibernation.
The beginning of the fateful experiments of Kelly Drew for Human hibernation
Every summer, Drew pitched a tent in the northernmost part of Alaska, called the North Slope, to trap arctic squirrels for his laboratory. The US Army Research Office funded his research; Because Drew had convinced them that the results of his research could be used to save severely injured soldiers by quickly and safely cooling their bodies on the battlefield. He told the military organization that he plans to identify the chemicals involved in hibernating arctic squirrels and then test whether these chemicals would have a similar effect on humans.
Read more: How could Big Bang arise from nothing?
Drew, who became an assistant professor at the Arctic Biology Institute in 1993, originally hypothesized that the neurotransmitter gamma-aminobutyric acid, known as GABA, was primarily responsible for hibernation in squirrels. GABA is essential for inducing sleep; It means the lowest level of metabolism for animals that are not able to hibernate. For example, our human metabolism typically drops by 15% when we sleep. On the other hand, hibernation, in all its complexity, is just a deep sleep; It means a state in which breathing is reduced, and appetite and elimination of waste materials are prevented. For example, bears do not defecate or urinate throughout their hibernation.
However, when Drew injected his squirrels with GABA and a host of related chemicals, they did not induce long-lasting, stable hibernation. Years passed like that, and by the time Drew celebrated his 40th birthday, his efforts to find the molecular key to hibernation had largely been fruitless.
In 2005, an undergraduate chemistry student named Benjamin Warlick started working as an assistant in Drew’s lab. One of Warlick’s tasks was to search the databases for new ideas about chemicals that might trigger hibernation in ground squirrels.
Among the papers Warlick found on hibernation, he came across an unknown paper from Japan’s Fukuyama University on golden hamsters that, although written entirely in Japanese, had a brief abstract in English. In this paragraph, it was mentioned that the article’s authors managed to wake up the golden hamsters from hibernation by injecting a drug that blocks the adenosine A1 receptor in the animal cells. Although the paper’s findings contradicted Drew’s research, Warlick sent it to his boss because he thought it was valuable.
Two years passed before Drew could send the entire article for translation. When he finally read the English version of this article in 2007, he had an idea. If blocking the adenosine A1 receptor (responsible for promoting sleep) wakes sleeping hamsters, perhaps activating them in its squirrels causes them to hibernate.
The key to the mystery of hibernation was in an unknown paper in Japanese.
And that’s exactly what happened; When Drew injected his squirrels with the adenosine A1-stimulating drug CHA, the squirrels’ body temperatures quickly dropped, and they went into hibernation. Of course, this happened only when the CHA drug was injected into them in the winter months. Therefore, there must have been something else going on in the brains of squirrels that prepared them for hibernation.
Although Drew was surprised by the effects of CHA on his squirrels, there were two major problems with using the drug; First, it had to be injected directly into the brain, which, well, sticking a needle into the human brain is rarely recommended, especially if it’s in a non-hospital setting. Second, when CHA enters the body, it engages the A1 adenosine receptors of the heart and slows down its heartbeat so much that it eventually stops beating. Consequently, using CHA in humans seemed possible only in very limited cases.
Now, almost 20 years have passed since the day Barnes put that frozen squirrel in Drew’s hands and planted the seeds of hibernation research in his mind, and Drew still hasn’t found a safe and effective way to induce hibernation in humans.
But then he came up with another idea: to mix CHA with another drug that would block its effect on the heart but still involve the brain. CHA is of the “agonist” type, which stimulates the receptors. But the medicine that blocks the nerve receptors is called an “antagonist.” Drew realized he needed an antagonist for adenosine A1 whose molecules were large enough to cross the blood-brain barrier (BBB).
Drew explains how agonists and antagonists behave in the body like this:
If you think of the body as a color map, so that the agonist is red, then red is spread throughout the body because it is stimulating all the receptors. We don’t want this agonist to stimulate cardiac receptors, So we need something to block these receptors. Now suppose the antagonist is blue. We add this to the body, but it’s not supposed to reach the brain. As a result, the whole body turns purple; But the brain is still red.
Adenosine A1 antagonists had been extensively researched, so Drew had several viable options. Finally, he chose the antagonist 8-(p-sulfonyl)theophylline, known as 8-SPT, which is closely related to one of the main ingredients of black tea. Drew decided to inject the 8-SPT and CHA into the abdominal area and conducted several experiments on mice to test the effectiveness of this combination.
The combined drug CHA/8-SPT induced hibernation in mice without complications.
Read more: Researchers find a way for creating Mars habitat
In these experiments, Drew stopped the heart of mice from moving and then brought them back to life by applying CPR. Once the mice were freed from death, one group was given the CHA/8-SPT combination drug, and the other group was left alone to allow their body’s metabolism to repair them at its normal rate. By conducting these experiments, Drew noticed that the mice that received the CHA/8-SPT combination had a better health status than the second group. And perhaps more importantly, the mice in the first group did not develop complications despite receiving the drug. There was no sign of shivering in these mice, and therefore there was no need to inject them with a sedative that would cause problems in their breathing.
Achieved on mice, patented the technique of using the CHA/8-SPT combination drug under the title “Methods and compositions for treating tissue damage by hypothermia”; And the first image he put on his patent form was that of a sleeping arctic ground squirrel, actually a reference to that small but fateful moment in 1992 that changed the course of his life forever.
How did Drew’s research reach NASA?
Familiar with science fiction films such as A Space Odyssey and Planet of the Apes, Drew vaguely knew that his research might one day attract the attention of the space exploration industry. Therefore, he was not surprised when he was contacted by NASA Spaceworks in February 2015. The company had just received funding to advance human hibernation research, and John Bradford invited Drew to join Spaceworks as a senior hibernation consultant.
Drew accepted Bradford’s invitation and soon began testing the CHA/8-SPT combination drug in pigs with anesthesiologist Matthew Kumar. The drug safely lowered pigs’ internal temperature to 30 and 32 degrees, not as much as doctors lower body temperature by intravenous fluids, but close enough.
Meanwhile, University of Colorado biologist Sandy Martin was also researching hibernation. Martin remembers those days:
I thought to myself that what we should do is understand how hibernating animals do this so beautifully and naturally without the slightest harm to their bodies. They don’t even need to use tubes for breathing and feeding.
Martin and his daughter began working on their paper, suggesting several promising avenues for research based on Martin’s genomic analysis of the leopard ground squirrel (a close relative of the arctic ground squirrel). One of the proposed methods was to further investigate a receptor called TRPM8, which plays a very important role in helping leopard squirrels regulate their body temperature during hibernation.
NASA could start injecting CHA/8-SPT in humans as early as 2026
In March 2018, NASA invited Drew, Martin, and a handful of leading hibernation researchers to attend a two-day conference in Mountain View, California; The event was named the first “Space Sleep Workshop.” This conference was a golden opportunity for biologists to convince NASA that with enough funding, they could help humans achieve some degree of hibernation in the next 10 to 15 years. Their timeline matched well with NASA’s plans to send humans to Mars in the late 2030s or early 2040s.
Speaking to NASA officials in this workshop, Martin emphasized that the frequency of hibernation among mammals shows that humans can also achieve it. There are three types of mammals in the animal world: egg-laying monotremes, such as platypus; Marsupials that raise their babies in pouches attached to their bodies, such as kangaroos; And finally, the group of couples that includes us, humans. Martin says:
In all three categories of mammals, there is a species that can hibernate. The simplest explanation for this is that the common ancestor of all three of us was hibernating.
Assuming Martin is right, then all we need to do to deal with humans’ physiological stresses of hibernation is a small genetic change.
Now, NASA accepts that hibernation is critical to making the spacecraft lighter and accepts Bradford’s view that hibernation can solve some of the physical problems astronauts face during long space trips.
Drew is now 63 years old and can’t believe he has spent nearly half his life figuring out the secret of squirrel hibernation. But thanks to the academic research of researchers like Drew, the private sector has also realized the potential of this field. For example, Silicon Valley startup FaunaBio aims to improve treatments for heart and lung diseases by discovering why hibernators survive in stressful conditions that are fatal for most humans.
Hibernation won’t just be for astronauts
If hibernation can one day become a realistic option for humans, even normal people who are not planning to travel to the Red Planet or are in good health could reap the benefits of a long sleep. Earlier this year, a group of UCLA researchers concluded that “the molecular and physiological responses required for hibernation in humans may reverse the aging process.”
Via: Wired


You may like
Many mental disorders have physical roots
Jessica Huston’s tics started when she was just 12 years old. Over time, his condition worsened until he had a seizure and was rushed to the hospital. Doctors at a local hospital in Durham, England, dismissed his condition and said he was suffering from anxiety and probably spent a lot of time watching TikTok videos.
Jessica actually suffers from an autoimmune disease caused by a streptococcal bacterial infection. His illness was a form of pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS). When the infection was identified and treated, her symptoms eventually began to improve.
Ms. Huston is not the only person with a brain dysfunction that is mistaken for a mental disorder. A lot of evidence shows that a series of infections can cause conditions such as obsessive-compulsive disorder, tic, anxiety, and even psychosis. Inflammatory and metabolic disorders can also have significant effects on mental health, although they are rarely considered by psychiatrists.
Rethinking the cause of mental disorders could have profound implications for the millions of people with mental illnesses who are currently undertreated. For example, more than 90% of patients with bipolar disorder develop recurrent illnesses during their lifetime. More than 46% of children with obsessive-compulsive disorder do not recover. About 50 to 60 percent of patients with depression eventually recover after trying different drugs. A deeper understanding of the biological components of mental health can lead to more accurate diagnoses and more targeted treatments.
Infections can cause obsessive disorder, tic, anxiety, and even psychosis
For a long time, the field of psychiatry has focused on describing and classifying symptoms rather than on underlying causes. The Diagnostic and Statistical Manual of Mental Disorders (DSM) was published in 1952 and contains descriptions, symptoms, and diagnostic criteria. Although this guide has helped unify diagnoses, it groups patients without considering the underlying mechanisms of mental disorders.
There is a lot of overlap between the symptoms of depression and anxiety, and some question whether they are really separate illnesses. At the same time, depression and anxiety exist in different forms. For example, panic disorder with and without agoraphobia are different diagnoses, but we may not find significant differences between them. This can lead to a high diversity of patients participating in drug trials, and these trials do not achieve results due to the few commonalities and large differences among the participants.
Previous attempts to find causal mechanisms for mental illness have been challenging. In 2013, the National Institute of Mental Health tried to distance itself from research based on classifications based on DSM symptoms. Huge budgets have been spent on research into brain disease processes with the hope of linking genes directly to behaviors. But this idea ultimately failed and most of the genes discovered had small effects.

Although genes may play a role in mental disorders, they are not the only answer. Many disorders such as schizophrenia, attention deficit hyperactivity disorder, anxiety, and autism can be caused by genetic disorder 22q11.2, in which part of chromosome 22 is deleted, says Ludger Tebartz van Elst, professor of psychiatry and psychotherapy at Freiburg University Hospital in Germany.
In 2007, studies conducted at the University of Pennsylvania showed that 100 patients with psychiatric symptoms or cognitive deficits actually had some kind of autoimmune disease. Their bodies were making antibodies against a key receptor in nerve cells called the NMDA receptor. This leads to swelling of the brain and can cause a wide range of symptoms including paranoia, hallucinations, and aggression. The disease described was called anti-NMDA receptor encephalitis, and in many cases, it was treatable by removing the antibodies or using immunotherapy drugs or steroids. Studies conducted on patients who had the first episode of psychosis have shown that between 5 and 10 percent of them also had antibodies that attack the brain.
It seems that in rare cases obsessive-compulsive disorder can also be caused by the immune system. This condition is seen in childhood PANDAS, which Ms. Houston was diagnosed within 2021. This disorder is sometimes seen in adults as well. A 64-year-old man spent a lot of time mowing his lawn, but the next day he felt remorse and guilt. The researchers found that these symptoms are caused by antibodies attacking the neurons in his brain.
Recently, Belinda Lennox, director of the Department of psychiatry at the University of Oxford, conducted experiments on thousands of patients with psychosis. He has found antibodies in blood samples of about 6% of patients, which mainly target NMDA receptors. He says it’s not clear how a set of antibodies can cause clinical symptoms ranging from seizures to psychosis to encephalitis. It’s also not clear why these antibodies are made or if they can cross the blood-brain barrier (the membrane that controls access to the brain). He hypothesizes that antibodies cross the blood-brain barrier and affect memory by binding to the hippocampus, leading to delusions and hallucinations.
Studies have shown that some patients with psychological symptoms or cognitive defects have some kind of autoimmune disease
Dr. Lennox says a medical rethink is needed to understand the damage the immune system can do to the brain. He is conducting experiments in this field.
Studies of patients with immune-mediated psychosis show that a wider range of strategies, including the removal of antibodies and the use of immunotherapy drugs or steroids, can be effective treatments.
People with myalgic encephalomyelitis/chronic fatigue syndrome (an infectious disease associated with a range of cognitive problems such as difficulty concentrating and paying attention) were once neglected or diagnosed as retarded. New research shows that myalgic encephalomyelitis is related to both immune disorders and metabolic disorders.
Metabolic disorders can also affect mental health. The brain is an extremely energy-demanding organ, and metabolic changes related to energy pathways are involved in various disorders, including schizophrenia, bipolar disorder, psychosis, eating disorders, and major depressive disorder.

At Stanford University, there is a metabolic psychiatry clinic where patients are treated with diet and lifestyle changes along with medication. An active area of research at this clinic is the potential benefits of a ketogenic diet, where carbohydrate intake is limited.
A ketogenic diet forces the body to burn fat for energy, creating chemicals known as ketones, which can be used as a fuel source in the brain when glucose is limited.
Metabolic disorders can affect mental health
Thirteen trials are underway around the world to examine the effects of metabolic therapies on serious mental illness, says Kirk Nylen, head of neuroscience at the US charity Bazoski Group, which funds brain research.
The preliminary results have shown that a large group of patients respond to these treatments in a meaningful way. Medicines, talk therapy, brain magnetic stimulation, and maybe electroshock therapy have not been effective for this group of patients.
It is not just the understanding of the immune and metabolic systems that is improving. Massive amounts of data are now being analyzed at unprecedented speed to reveal connections that were previously hidden from view. This could ultimately lead to more personalized and better treatments.
In early October 2023, the UK Biobank published data showing that people with depressive episodes had higher levels of inflammatory proteins such as cytokines in their blood. According to another study, about a quarter of depressed patients showed evidence of mild inflammation. Knowing this can be helpful because other research shows that patients with inflammation respond poorly to antidepressants.
There are new advances in understanding the underlying causes of mental disorders. A group of researchers are investigating different ways to improve the diagnosis of ADHD; Like classifying patients into different subgroups, some of which were previously unknown. Different groups of researchers announced in three different statements in February 2024 the discovery of biomarkers that can predict the risk of dementia, autism, and psychosis.
The search for better diagnostic tools is also likely to be accelerated by the use of artificial intelligence. A company called Cognoa is using artificial intelligence to diagnose autism in children by analyzing videos of their movement behaviors in doctors’ waiting rooms.
The Quantitative Biosciences Institute (QBI) in California has used artificial intelligence to create an entirely new map of the interactions between proteins and molecular networks involved in autism. This will greatly facilitate finding diagnostic and therapeutic tools.
The developments mentioned are promising. But many problems can be solved by reducing the gap that exists today between neurology and psychiatry. Neurology studies and treats physical, structural, and functional disorders of the brain, while psychiatry deals with mental, emotional, and behavioral disorders. Dr. Lennox envisions a future in which antibody testing is performed when a person who develops a sudden mental breakdown after a viral infection fails to recover with standard treatments.
According to Dr. Tebartz van Elst, the gap between neurology and psychiatry is greater in Anglo-Saxon countries (including the United States, Great Britain, Canada, and New Zealand). In Germany, psychiatry and neurology are closer together, so neurologists are trained in psychiatry and psychiatrists are trained in neurology for one year. This makes research work easier.
For most patients who are first diagnosed with psychosis or other severe psychiatric syndromes, Dr. Tebartz van Elst prescribes brain MRIs, electroencephalograms, laboratory tests for inflammation, and lumbar punctures in order to better treat them by finding clues to the cause of the illness. Submitted.


Why do people listen to sad songs?
There is a paradox in sad music: we don’t enjoy sadness in real life, but we enjoy art that makes us feel that way. Countless researchers since Aristotle tried to solve this contradiction. Perhaps through music, we experience a kind of catharsis of negative emotions. Catharsis here means refinement and cultivation of the soul. Maybe there is an evolutionary advantage in this feeling of sadness, or maybe we want to value our suffering. Maybe our body produces hormones in response to anxiety disorder, music that leads to a sense of comfort.
According to the New York Times, Dr. Nob, an experimental philosopher and psychologist at Yale University, in a new study published in the Aesthetic Education Journal, raised the question, “What is the purpose of sad music?” He tried to solve the contradiction of this kind of music. Over the years, he came to the conclusion that people often have two perceptions of the same thing. For example, they can consider people as artists if they have a set of characteristics such as an innate talent for working with a brush; But if they don’t have abstract values such as creativity, curiosity or interest and just recreate old masterpieces for profit, we can say they are not artists. According to Dr. Nob and his former student Tara Venkatsan, a cognitive scientist, perhaps sad music also has a dual nature.

The aforementioned research shows that our emotional response to music is multidimensional; You don’t necessarily feel happy when you listen to a beautiful song, and you don’t necessarily feel sad when you listen to a sad song. According to a 2016 study, the emotional response of 363 listeners to sad songs was divided into three categories: sadness and strong negative emotions such as anger, panic, and despair, nostalgia, quiet sadness and self-compassion, and finally sweet sadness is pleasant pain. It comes from consolation and understanding. Many respondents reported a combination of all three. The researchers called this research “Fifty Blue Spectrums”.
Given the layers of emotion and the ambiguity of language, it’s no wonder that sad music creates a paradox; But it is not clear why it induces a sense of pleasure or meaning. Some psychologists have investigated how certain aspects of music, such as position, pitch, rhythm, and resonance, are related to listeners’ emotions. According to research, certain forms of songs have an almost universal function: for example, among different countries and cultures, lullabies have similar acoustic characteristics that make children and adults feel safe. Thomas Irola, a musicologist at the University of Durham in England and researcher of the “Fifty Spectrum” study, says:
Throughout life, we learn to make connections between our feelings and what we hear. We recognize emotional expression in speech, and often these cues are used in a similar way in music.
Other researchers, such as Patrick Joslin, a music psychologist from Uppsala University in Sweden, believe that such findings reveal the value of sad music. Sad music, he writes in an essay, asks why “the second movement of Beethoven’s Eroica symphony evokes a sense of sadness?” It leads to the question, “Why does a slow step lead to a feeling of sadness?”
According to the findings of Joslin and his colleagues, there are cognitive mechanisms through which feelings of sadness are induced in listeners. These mechanisms include unconscious reactions in the brain stem, synchronization of the rhythm with the internal rhythm such as the heartbeat, conditional reactions to certain sounds, the arousal of memories, emotional contagion, and reflexive measurement of music. Perhaps because sadness is such a strong emotion, it can evoke an empathetic and positive response. In fact, understanding other people’s grief provokes a social response.
Why do people listen to sad songs?
The purpose of listening to sad music is not necessarily to convey sadness; Rather, it is creating a sense of connection.
Dr. Nob, along with Dr. Venkatsan and George Newman, a psychologist at the Rotman School of Management, designed a two-stage experiment to test the hypothesis. In the first part of the experiment, they gave one of four song descriptions to more than 400 participants. In the description of the first song, it was written: “transmitting complex and deep emotions, but technically full of errors.” The second track was described as: “music without technical errors that do not convey complex and deep emotions.” The third song was described as “highly emotional and technically flawless” and the fourth song was described as “technically flawed and non-emotional”.

Subjects were asked to indicate on a seven-point scale whether their song conveyed the intent of the music or not. Their goal was to show how important it is for music to express emotion and generally happiness, sadness, hate, or any other emotion on an intuitive level. Overall, subjects reported that deeply emotional but technically flawed songs best reflected the nature of music. In other words, the emotional expression had a more prominent value than the technical aspect.
In the second part of the experiment, which included 450 new subjects, the researchers gave each participant 72 descriptions of emotional songs that convey feelings such as “humiliation,” “narcissism,” “inspiration,” and “lust.” For comparison, they gave participants phrases that convey conversational interaction in expressing people’s feelings. For example, one of the phrases was: “An acquaintance is talking to you about the past week and his feeling of passion”. In general, the emotions that the subjects receive are strongly rooted in the “purpose of the music” and are similar to the emotions that make people feel close to each other in conversation: emotions such as love, joy, loneliness, sadness, ecstasy, and relaxation.
Mario Etti Picker, a philosopher at Lowell University of Chicago, finds the results of this study interesting. After reviewing the data, he came up with a relatively simple idea: “Perhaps the reason we listen to music is not just an emotional response, but we do it to understand the connection with others; Because, according to the reports of many subjects, sad music is not necessarily enjoyable despite its artistic dimensions. In other words, according to the paradox of sad music, our love of music is not the result of direct praise of sadness; Rather, it is the result of valuing communication with others.”
Dr. Irola also concluded in his research that empathic people are likely to be moved by unfamiliar sad music. They tend to engage in this kind of imaginary grief. These people also show significant hormonal changes in response to sad music. But sad music, like an onion, has many layers, and this explanation can give rise to other questions. For example, who should we communicate with? Artist or with our own past? Or even with an imaginary person?
A new drug developed to treat severe influenza works in a unique way, unlike what a drug would expect, to treat lung disease and infection.
Inventing a new drug to treat influenza!
A new drug to treat severe flu successfully keeps patients at the right level of lung inflammation to protect against lung damage while still allowing the immune system to fight infection. This drug has been effective in mice even a few days after infection.
According to New Atlas, if you’ve ever had the flu, you’ve most likely contracted the influenza A virus (IAV). Compared to influenza B virus, infection with type A often causes more severe symptoms. But, while many of us have experienced the fever and chills, headache and muscle aches, fatigue, sore throat, and cough of the common flu, severe infection with the animal IAV strain is different and potentially life-threatening.
Severe infection of this type of influenza causes a special type of cell death called necroptosis in infected cells. While this is a natural process designed to limit viral spread by actively eliminating infected cells and mobilizing the immune system to respond, necroptosis can activate a hyperinflammatory response and cause collateral lung damage that is potentially fatal. Is. Other than managing its symptoms, there are few treatment options for treating severe influenza.
In a new study, researchers from Tufts University School of Medicine, St. Jude Children’s Research Hospital, the University of Houston, and Fox Chase Cancer Center collaborated to test a drug called UH15-38 that could prevent this flu-related lung damage in mice. It prevents and allows the immune system to fight the virus.
“Our drug significantly increased survival and reduced symptoms of influenza virus infection,” said Paul Thomas, co-author of the study. The new drug reduced dangerous inflammation and even seemed to improve the adaptive response to the virus.
Achieving the Goldilocks effect, or the effect of the right amount of the drug on inflammation, required researchers to use clever chemistry along with a thorough understanding of the underlying mechanisms of necroptosis.
Receptor-interacting protein kinase 3 (RIPK3) is an essential part of the necroptosis cell death pathway, but it also controls another cell death pathway called apoptosis. Both types of cell death trigger opposing immune responses. Apoptotic death usually results in muted immunological responses, while necroptosis releases molecules that cause inflammation. UH15-38 was designed to prevent the stimulation of the necroptosis pathway by RIPK3, while still allowing cell death and removing infected cells in a less inflammatory manner.
Alexei Degterev, an associate professor of developmental, molecular, and chemical biology at Tufts University School of Medicine and one of the authors of the paper, says: “If you eliminate necroptosis, you will still limit virus replication without severe damage to the lungs.” Necroptosis does not appear to be necessary to limit viral activity, so if we can block it, we can protect the host by reducing inflammation in the lungs.
Read more: Testing a vaccine that reduces liver tumors
The researchers tested the drug UH15-38 in mouse models and found that high doses of the drug provided protection against the usually fatal IAV influenza. At low doses, the UH15-38 drug protected mice against similar amounts of influenza that humans experience. Notably, the mice were protected even if they received the drug several days after being infected with the disease.
“This drug can do something we haven’t seen before,” says Thomas. We can start five days after the initial infection and still see benefits. Completely removing the RIPK3 protein is not a great choice because then the immune system cannot clear the virus. When we removed only the necroptosis, the animals did better because they still had apoptosis and could still get rid of the infectious cells, but their condition was not as severely inflammatory.
UH15-38 improved survival by preventing collateral necroptosis damage to type 1 alveolar epithelial cells, a special type of cell in the lungs that facilitates gas exchange. Damage to these cells can make it difficult for oxygen to enter the blood and carbon dioxide from it, and cause symptoms such as shortness of breath, wheezing, and chest tightness. The drug also reduced the number of immune cells associated with inflammation, such as neutrophils, in the mice.
Often, the worst part of the flu happens after the virus is under control when inflammation destroys lung cells, Thomas says. UH15-38 can reduce influenza-induced inflammation while leaving viral clearance and other functions of tissue and immune responses intact. This makes the drug a promising option to move towards clinical use.
The next step is clinical and human trials safely. Researchers are testing whether UH15-38 is effective in treating other respiratory diseases.
While the worst of COVID-19 may be upon us, another pandemic is expected, and we need something that protects the host regardless of how it is infected, Degtref says. This study demonstrates the possibility of achieving such a goal and renews interest in how cell death occurs against infections.
This study was published in the journal Nature.


MacBook Air M3 review; Lovely, powerful and economical


How to prevent the earth from being baked by the scorching sun?


James Webb space telescope map of the climate of an exoplanet


The highest observatory in the world officially started its work


Many mental disorders have physical roots


Asus Zenbook 14 OLED laptop review


The secret of the cleanest air on earth has been discovered


How extinct animals could be brought back from death?


Xiaomi Pad 6S Pro review


Testing a vaccine that reduces liver tumors
Popular
-



 Technology9 months ago
Technology9 months agoWho has checked our Whatsapp profile viewed my Whatsapp August 2023
-



 Technology10 months ago
Technology10 months agoHow to use ChatGPT on Android and iOS
-



 Technology9 months ago
Technology9 months agoSecond WhatsApp , how to install and download dual WhatsApp August 2023
-



 Technology11 months ago
Technology11 months agoThe best Android tablets 2023, buying guide
-


 Humans1 year ago
Humans1 year agoCell Rover analyzes the inside of cells without destroying them
-



 AI1 year ago
AI1 year agoUber replaces human drivers with robots
-



 Technology10 months ago
Technology10 months agoThe best photography cameras 2023, buying guide and price
-



 Technology11 months ago
Technology11 months agoHow to prevent automatic download of applications on Samsung phones