The relationship between schizophrenia and mother’s vitamin D! Researchers have used molecular imaging technology to confirm the role of vitamin D in the early development of brain cells and say that the origin of schizophrenia may be related to the amount of vitamin D in the mother’s body.
The relationship between schizophrenia and mother’s vitamin D!
In this article we’re going to read about the relationship between schizophrenia and mother’s vi Researchers have used molecular imaging technology to confirm the vital role of vitamin D in the mother’s body for the development of brain cells that produce dopamine, the feel-good chemical in the body.
This finding provides a greater understanding of the underlying mechanisms of neurodevelopmental disorders such as schizophrenia.
Schizophrenia is thought to be caused by a combination of genetic and environmental factors. The exact mechanism by which it does this is unknown, but there is strong evidence that this condition changes the way the brain uses dopamine.
Read More: The promising effect of a smart virus in the treatment of invasive brain cancer
Scientists hypothesize that exposure to risk factors for schizophrenia during fetal development changes the way dopamine circuits are formed in the brain. Previous studies have shown that low levels of vitamin D in the mother’s body are one of the risk factors that affect the differentiation of dopamine-producing (dopaminergic) neurons into their specialized and mature form.
Now, a group of researchers at the Brain Institute of the University of Queensland, based on past research and with the help of molecular imaging technology, have investigated more closely the relationship between vitamin D, dopaminergic neurons, and schizophrenia.
Scientists created dopamine-like neurons to replicate the differentiation process that occurs during embryonic development. Then these neurons were cultured with and without calcitriol hormone.
Digested vitamin D is inactive until it undergoes two enzymatic reactions in the body. The second reaction occurs in the kidney, where it is converted to calcitriol, the active form of vitamin D. Calcitriol binds to the vitamin D receptor in the cell nucleus and activates it.
Researchers found that vitamin D not only affects cell differentiation but also neuron structure.
“What we found was that the altered differentiation process in the presence of vitamin D not only caused the cells to grow differently but also recruited the machinery to release dopamine differently,” said lead author Daryl Eales.
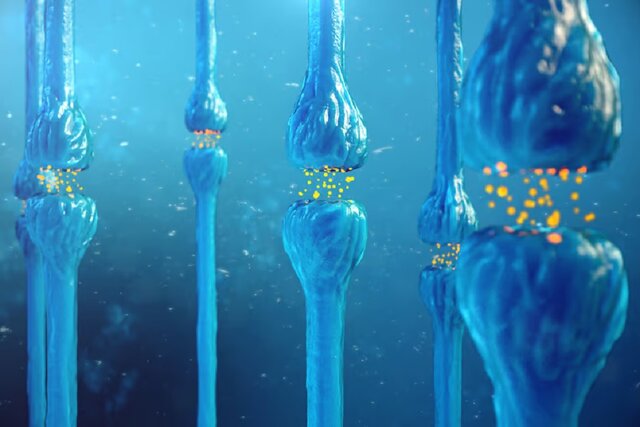
What these machines mean are neurites, the projections that grow from the cell body of a neuron. Neurites need to send and receive signals to and from other parts of the nervous system.
The researchers found that the number of neurites increased significantly, and in those neurites, the distribution of proteins responsible for the release of dopamine changed. Using a new imaging tool called pseudo-fluorescent neurotransmitters (FFNs), scientists can study how dopamine uptake and release changes in the presence or absence of calcitriol.
FFNs are small molecule dyes that mimic the action of a neurotransmitter such as dopamine. They allow imaging of the storage and release of single molecules in nerve terminals.
The researchers found that compared to the control group, dopamine release was increased in neurons grown in the presence of calcitriol.
“Vitamin D certainly affects the structural differentiation of dopaminergic neurons,” Eales says.
Using FFN to target and observe dopamine molecules means researchers can confirm their long-held belief that vitamin D levels during development affect how dopamine-producing neurons form.
They believe that early changes in dopamine neuron differentiation and function may lead to the dopamine dysfunction seen in adult-onset schizophrenia.
Schizophrenia is a mental disorder characterized by persistent or recurrent episodes of psychosis. Its main symptoms include hallucinations (often auditory hallucinations), delusions, and thought disorders. Other symptoms include social withdrawal, decreased emotional expression, and apathy.
These symptoms usually develop gradually, starting in early adulthood, and in many cases never completely resolve.
There is still no specific test to diagnose it, and it is only diagnosed based on the behavior observed by the patient by a doctor or clinical psychologist along with a history including the reported experiences of the person and the reports of people familiar with the person.
In order to diagnose schizophrenia, doctors must confirm that symptoms and functional disorders have existed in a person for six months. Many people with schizophrenia also have other mental disorders, especially substance abuse disorders, depressive disorders, anxiety disorders, and obsessive-compulsive disorder.
About 0.3 to 0.7% of people are diagnosed with schizophrenia during their lifetime. Estimates in 2017 indicated 1.1 million new cases and in 2019 there were a total of 20 million cases of this disease in the world.
Men suffer from schizophrenia more than women, and the age of onset of the disease in men is on average lower than in women; Although some extensive research has not found gender differences in the prevalence of this disorder.
Possible causes of schizophrenia include genetic factors and environmental factors. Genetic factors include common and rare genetic variants. Possible environmental factors include growing up in the city, marijuana use during puberty, infections, the age of the mother or father, and poor maternal nutrition during pregnancy.
About half of people with schizophrenia make a significant long-term recovery without relapse, and a small proportion of these people recover completely. But the remaining 50% will be disabled for life. In some cases, a person may be hospitalized repeatedly.
Social problems such as long-term unemployment, poverty, homelessness, and abuse of patients and victims are common. The average life expectancy of people with this disorder is 20 years less than the general population. This problem is the consequence of increased physical health problems and a higher suicide rate (about 5%) in schizophrenia patients.
It is estimated that in 2015, around 17,000 people around the world died due to factors related to or caused by schizophrenia.
The main core of the treatment of this disease is the use of antipsychotic drugs, along with psychotherapy, job training, and social rehabilitation. Up to one-third of patients may not respond to first-generation antipsychotics, in which case a second-generation antipsychotic such as clozapine may be used. In situations where doctors determine that there is a risk of harming oneself or others, short-term mandatory hospitalization may be prescribed. Long-term hospitalization is used only in a small number of severe cases of schizophrenia. Longer hospital stays are observed in some countries where supportive services are limited or unavailable.
Finally, schizophrenia is a mental disorder characterized by significant changes in perception, thoughts, behavior, and mood. Schizophrenia symptoms are divided into three categories: positive, negative, and cognitive symptoms. Positive symptoms of schizophrenia are symptoms that are common in other psychotic illnesses and are sometimes referred to as psychotic symptoms. These symptoms may be present in any of the different psychotic disorders, and because they are often transient, they make early diagnosis of schizophrenia difficult.
Now the researchers of the new study plan to investigate whether other environmental risk factors for schizophrenia, such as low oxygen levels or infection during pregnancy, also change the way dopamine neurons develop.
This study was published in the journal Neurochemistry.



 Technology9 months ago
Technology9 months ago


 Technology10 months ago
Technology10 months ago


 Technology9 months ago
Technology9 months ago


 Technology10 months ago
Technology10 months ago

 Humans1 year ago
Humans1 year ago


 AI1 year ago
AI1 year ago


 Technology10 months ago
Technology10 months ago


 Technology10 months ago
Technology10 months ago